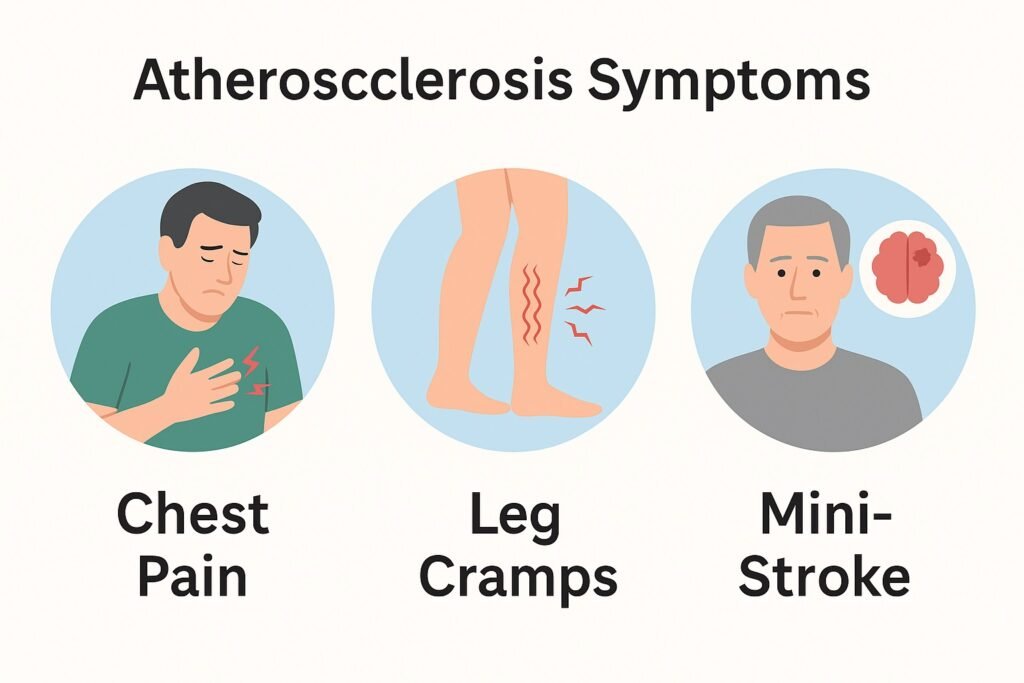
Understanding atherosclerosis symptoms early can prevent heart attack, stroke, and limb complications. Learn the subtle warning signs, how they differ by artery, and when to seek medical help.
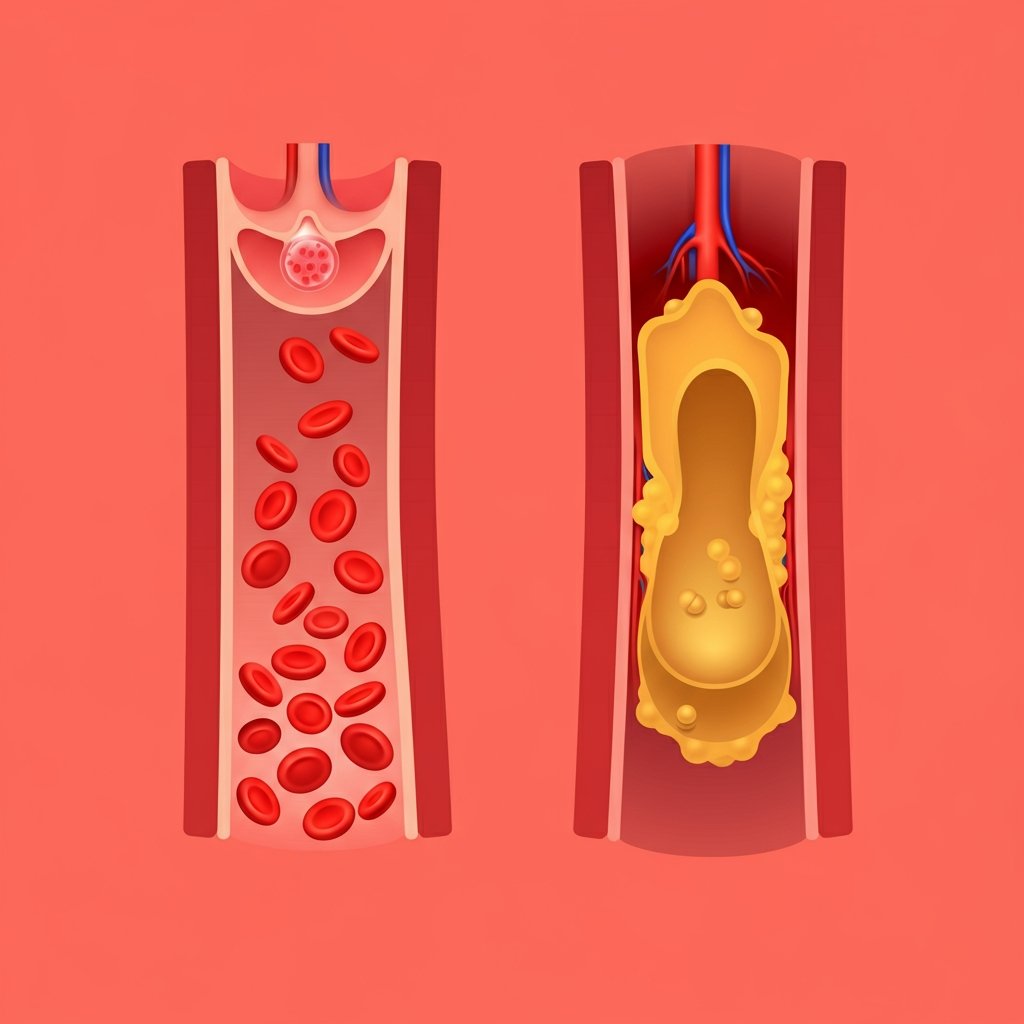
Atherosclerosis symptoms often start quietly. Plaque builds inside the arteries, narrowing blood flow until the heart, brain, or limbs don’t receive enough oxygen—then symptoms appear, sometimes suddenly. Recognizing these early warning signs helps you act before a heart attack, stroke, or critical limb problem occurs.
Key point: Mild or infrequent symptoms—like chest pressure on hills, or calf cramps that stop with rest—can still signal atherosclerosis. Don’t wait for severe pain to get evaluated.
What Is Atherosclerosis?
Atherosclerosis is the gradual accumulation of fatty deposits (plaque) within artery walls. Over time, plaques harden or rupture, restricting blood flow or forming a clot that abruptly blocks the artery. This process can affect many vascular beds, so symptoms depend on which arteries are involved.
- Coronary arteries (heart) → chest discomfort, shortness of breath, fatigue with exertion.
- Carotid or cerebral arteries (brain) → transient ischemic attacks (TIAs), stroke-like symptoms.
- Peripheral arteries (legs/feet) → cramping with walking, cold feet, slow-healing wounds.
- Renal arteries (kidneys) → difficult-to-control blood pressure, kidney function decline.
Key Atherosclerosis Symptoms by Location
1) Heart (Coronary Artery Disease)
When plaques narrow the coronary arteries, the heart muscle receives less oxygen during exertion. Typical symptoms include:
- Chest pressure or tightness (angina), often with activity or stress; may radiate to arm, neck, jaw, or back.
- Shortness of breath, reduced exercise capacity, unusual fatigue.
- Indigestion-like discomfort that doesn’t clearly relate to food.
Emergency: New, severe, or persistent chest pain; pain at rest; sudden sweating or nausea—call emergency services immediately.
2) Brain (Carotid/Cerebral Arteries)
Narrowing or clot in arteries to the brain can cause transient ischemic attacks (TIAs) or strokes:
- Sudden weakness or numbness in the face, arm, or leg—often one side of the body.
- Difficulty speaking or understanding speech; sudden confusion.
- Sudden vision changes (one eye or both), dizziness, severe headache, loss of balance.
Act FAST: Face drooping, Arm weakness, Speech difficulty, Time to call emergency.
3) Legs & Feet (Peripheral Artery Disease, PAD)
Reduced blood flow to the legs causes classic claudication—cramping pain with walking that resolves with rest. Other signs:
- Foot/toe wounds that heal slowly or not at all.
- Cold feet, reduced hair growth on shins, brittle nails, pale or bluish skin.
- Pain at rest in advanced disease (critical limb ischemia).
4) Other Territories
- Renal arteries: resistant hypertension, fluid retention, kidney function decline.
- Mesenteric arteries: abdominal pain after meals, unintentional weight loss.

Early Warning Patterns You Shouldn’t Ignore
- Predictable chest pressure on hills/stairs that eases with rest.
- Calf cramps after a set distance, relieved by pausing.
- Brief neurologic episodes—slurred speech, one-eye vision loss—that resolve within minutes (possible TIA).
- Slow-healing foot sores or color/temperature changes in toes.
- Disproportionate fatigue during normal activities.
Tip: Keep a symptom diary: what you were doing, duration, recovery time. This helps your clinician choose the right tests.
Who Is at Higher Risk?
Certain conditions accelerate plaque buildup and make atherosclerosis symptoms more likely:
- High LDL cholesterol or triglycerides; low HDL.
- High blood pressure, diabetes, chronic kidney disease.
- Smoking (active or past), secondhand smoke exposure.
- Obesity, sedentary lifestyle, poor diet quality.
- Family history of early cardiovascular disease.
- Age (risk increases after ~45 in men and ~55 in women).
Having multiple risk factors compounds risk. The earlier you address them, the more you can prevent complications.
How Atherosclerosis Is Diagnosed
Your clinician will tailor tests to your symptoms:
| Test | What it checks | Common uses |
|---|---|---|
| Blood tests | Lipids (LDL, HDL, triglycerides), glucose/A1C, kidney function | Risk assessment and treatment targets |
| ECG & Echocardiogram | Rhythm, heart structure, and function | Coronary disease evaluation; HCM exclusion |
| Exercise Stress Test | Heart response to exertion | Detects exertional ischemia |
| Coronary Calcium Score (CT) | Calcium in coronary arteries | Refines risk in intermediate-risk adults |
| Ultrasound (Carotid/Leg) | Flow velocity and plaque | TIAs/stroke risk; PAD severity |
| Ankle–Brachial Index (ABI) | Leg blood flow vs. arm | Screening for PAD |
| CT/MR Angiography | Detailed vessel imaging | Complex cases and pre-intervention planning |
Treatment Overview (Brief)
While this article focuses on atherosclerosis symptoms, knowing the basics of management helps you connect symptoms to action:
- Lifestyle: Mediterranean-style eating, regular aerobic exercise, tobacco cessation, sleep, stress management.
- Medications: statins (LDL lowering), antiplatelets (per your clinician), ACE inhibitors/ARBs, diabetes and blood pressure control.
- Procedures: angioplasty/stent, endarterectomy, or bypass in selected cases.
Good news: Many symptoms improve when risk factors are controlled and physical activity is introduced gradually under medical guidance.
When to Seek Medical Care
- Immediately: severe chest pain, symptoms of stroke (FAST), sudden shortness of breath, or fainting.
- Within days: new exertional chest pressure, progressive leg cramps with walking, slow-healing foot wounds.
- Routine visit: you have risk factors and want to screen before symptoms escalate.
Related Reading & Internal Links
Continue learning with these guides on our site:
- Prevention – Lifestyle: practical steps to lower risk.
- Healthy Diet: heart-friendly foods and weekly meal ideas.
- Causes – Risk Factors: what drives plaque formation.
- Treatments – Remedies: from medications to procedures.
Trusted External Sources
Learn more from reputable organizations (editorial—do-follow recommended):
- Mayo Clinic – Atherosclerosis
- American Heart Association – Atherosclerosis
- World Health Organization – Cardiovascular Diseases
FAQs on Atherosclerosis Symptoms
What are the earliest atherosclerosis symptoms?
Subtle chest pressure with exertion, breathlessness, calf cramps on walks, and brief neurologic episodes can be early signs. Don’t ignore persistent or recurring symptoms.
Do atherosclerosis symptoms differ in women?
Yes. Women may have atypical coronary symptoms—shortness of breath, fatigue, indigestion, or back/jaw discomfort—without classic chest pain. The same urgency applies if symptoms are new or progressive.
Can symptoms improve without procedures?
Often, yes. Lifestyle changes and medication can reduce symptoms and future events. Procedures are reserved for specific cases or when symptoms persist despite optimal therapy.
Medical disclaimer: This article is educational and not a substitute for professional medical advice. If you suspect a medical emergency, call local emergency services immediately.




